A common misconception among people who are new to the low oxalate diet is that some people are sensitive to oxalate and others are not. This is definitely not true. Our bodies were designed to handle a small amount of oxalate. After all, we make oxalic acid as a natural part of our metabolism. But large amounts of oxalate are toxic to all animals, including humans, and will eventually compromise our health. The difference is some people accumulate high levels of oxalate in their bloodstream, urine and/or tissues, while others don’t. Why?
Top Six Reasons Why Some People Accumulate High Levels of Oxalate:
1.) Genetic Defects – Primary Hyperoxaluria Types I and II are caused by rare autosomal recessive diseases. In both types an enzyme in the liver is missing or defective, which causes people with PH to produce large amounts of oxalate. Doctors typically only diagnose primary hyperoxaluria in young patients (usually under 40) who present with severe kidney stones. Since all of the research surrounding primary hyperoxaluria has involved patients who form kidney stones, very little is known about whether people with other oxalate-related symptoms have these genetic defects. We do know that people with oxalate-related symptoms other than kidney stones respond to some of the same treatments given to people with milder forms of PH (drinking lots of water, taking vitamin B6, avoiding high oxalate foods, and taking citrate — usually calcium citrate), so it is possible that some of us (especially those of us with healthy gut function) have a genetic defect that causes our bodies to produce too much oxalate. If you are a kidney stone former, the Oxalosis and Hyperoxaluria Foundation is a good resource to find out more about PH. If you are not a kidney stone former, you will find this site frustrating although you may also gain some insight into your own treatment.
2.) Vitamin B6 Deficiency – People who have a vitamin B6 deficiency produce greater amounts of oxalate than people who do not have a deficiency. Vitamin B6 deficiencies may be related to a genetic defect such as PH described above, a lack of adequate B6 in the diet, vitamin absorption issues in the intestines, birth control pills, lactation and pregnancy, vitamin metabolism issues, collagen disorders, drug interactions or cancer, among other potential mechanisms. This is why many people on a low oxalate diet supplement with B6 or a B-complex vitamin, often at high levels (B1 and B5 deficiencies may also cause excess oxalate production which is why a B-complex is sometimes used).
3.) Poor Intestinal Health and Function – A healthy, well-functioning gut provides an effective barrier to the absorption of excess oxalate from the diet. Unfortunately, many things can go wrong with our intestines including inflammation; irritation of the gut lining; a reduced microflora (often from antibiotic use) or an unbalanced microflora (dysbiosis); fat malabsorption (steatorrhea); leaky gut (permeable intestines); scarring, reduced intestinal length or ileal bypass following injury or surgery; and disease, such as celiac sprue, Crohn’s disease and ulcerative colitis. Any of these intestinal issues can allow excess oxalate from the diet to be absorbed into the bloodstream. This is why many people on the low oxalate diet also take steps to improve their intestinal function, such as taking digestive enzymes, taking high-potency probiotics, eating fermented foods (like sauerkraut and yogurt) and eliminating gluten or all grains from their diets.
4.) High Levels of Oxalate in the Diet – People who don’t have one of the above three problems would have to eat a very high oxalate diet before they started to experience oxalate-related symptoms, but it can happen, especially with high consumption of rhubarb, spinach, almond or calallo0 (a green common in the West Indies). For those of us who do have one of the first three problems, eating too much oxalate is like adding fuel to the fire, especially if you have compromised gut health or gut function. If your intestines are not doing one of the intestines’ most important jobs – keeping toxic substances out of your body—then you must reduce the amount of oxalate (and all other toxins!) in your diet to begin the healing process (see Four Effective Approaches to the Low Oxalate Diet for tips on how to start a low oxalate diet and the Low Oxalate Diet Store for low oxalate foods and products).
5.) Mineral-Poor Diet – People who do not eat enough mineral-rich foods (especially calcium, magnesium, potassium and iron) absorb more oxalate than people who each mineral-rich diets. Most minerals readily bind with soluble oxalate (oxalic acid) in the intestines, forming insoluble oxalate salts which are not as easily absorbed through the intestinal wall (see What is Oxalate? for more information about oxalic acid and insoluble oxalate). This is why most low oxalate dieters take calcium citrate, magnesium citrate or Oxabsorb 20 minutes before meals—to help bind the oxalate before it can enter the bloodstream and cause a toxic effect. Many low oxalate dieters also incorporate mineral-rich bone broths into their whole foods cooking routine—both to bind with oxalate in the intestines and to counteract oxalate’s antinutrient effect (Just think–if calcium is binding with oxalate to form an insoluble salt that passes harmlessly out of your body, then not only is the oxalate not being absorbed, the calcium is not being absorbed either!). Although the role of minerals in your diet is important, it’s more likely that people have mineral deficiencies due to oxalate problems rather than oxalate problems due to mineral deficiencies.
6.) All of the Above! – The most common reason some people accumulate toxic levels of oxalate in their bodies is not one reason, but a combination of the above reasons. Although genetic defects are rare (or at least assumed to be rare by a medical community that is only testing kidney stone patients for the defect), the other four factors are quite common, especially in developed nations and Western cultures. I personally was deficient in B6 (possibly because of PH), had poor gut function due to overuse of antibiotics and consumption of irritating foods, and previously consumed a very high oxalate vegetarian diet, chock-full of spinach, almonds, chocolate and tea! My previous lifestyle was a recipe for an oxalate-related disaster.
Hope you enjoyed this overview of what causes some people to accumulate high levels of oxalate. Over the next few months, I hope to cover each of these reasons in more depth, especially intestinal function and intestinal health since I personally believe this may be the key to healing for most of us.
References and Resources:
1. Oxalosis and Hyperoxaluria Foundation
2. Low Oxalate Diet (Autism Research Institute)
3. Trying Low Oxalates
4. Savage, G. P., L. Vanhanen, S. M. Mason and A. B. Ross. 2000. Effect of cooking on the soluble and insoluble oxalate
content of some New Zealand foods. Journal of Food Composition and Analysis 13:201-206.
5. Henderson, J. M. and A. H. Merrill Jr. 1987. Diseases associated with defects in vitamin B6 metabolism or utilization. Annual Review of Nutrition 7 (1):137-156.
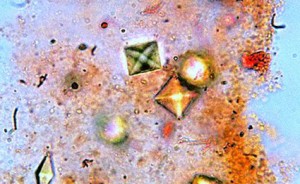
Photo credits go to Leboski for Sedemento 13 and to OliBac for Rhubarb 2.

{ 9 comments… read them below or add one }